COVID-19 Infection Linked to Increased Risk of Long-Term Brain Disorders

Emerging research reveals that COVID-19 infection may have lasting impacts on brain health, increasing the risk of neurological conditions such as stroke, depression, migraines, and anxiety.
Key Takeaways:
-
COVID-19 has been associated with a significant rise in neurological problems.
-
Over 40 million new cases of brain and nerve disorders may be linked to COVID-19 worldwide.
-
Preventing infection remains crucial for protecting long-term brain health.
Scientists are continuing to uncover the full extent of how COVID-19 impacts the brain and central nervous system. New findings published in Nature Medicine suggest that people who contract COVID-19 are at a 7% higher risk of developing neurological conditions compared to those who have never been infected.
According to Ziyad Al-Aly, MD, a clinical epidemiologist at Washington University in St. Louis, COVID-19’s neurological consequences go far beyond temporary brain fog. His team found associations between the virus and long-term complications like strokes, seizures, migraines, brain inflammation, and various mental health disorders.
Alarmingly, researchers estimate that COVID-19 may have contributed to more than 40 million new cases of neurological issues globally.
"We are seeing these brain problems not just in people who were severely ill, but even among those with mild infections," Dr. Al-Aly noted. "The risk extends across age, gender, and health status."
COVID-19 Raises the Risk for Numerous Brain Disorders
In the study, researchers reviewed the medical records of 154,068 U.S. veterans who tested positive for COVID-19 between March 2020 and January 2021. They compared their outcomes to over 11 million individuals without COVID exposure.
Their analysis revealed that within a year of infection:
-
Memory problems were 77% more likely
-
Stroke risk increased by 50%
-
Seizure risk rose by 80%
-
Mental health disorders became 43% more common
-
Headache risk jumped by 35%
-
Movement disorders, such as tremors, were 42% more likely
Importantly, even individuals who were not hospitalized for COVID-19 showed higher risks for neurological complications, highlighting the potential long-term consequences of even mild infections.
Researchers estimated that nearly 6.6 million Americans may have developed brain impairments due to COVID-19. These findings suggest potential long-term burdens on healthcare systems and broader economic impacts.
"The extent of the damage caused by COVID-19 to brain health was much more significant than we initially thought," said Dr. Al-Aly.
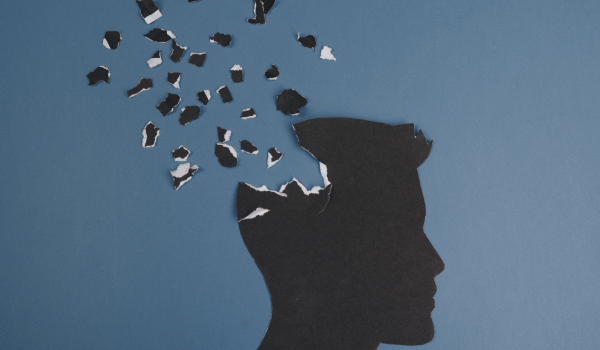
How COVID-19 Affects the Brain
Although the exact mechanisms remain unclear, several theories offer insight into how COVID-19 may lead to brain problems:
-
Inflammation: COVID-19 triggers widespread inflammation, which may harm the nervous system.
-
Vascular Damage: The virus can injure blood vessels that supply the brain, leading to impaired brain function.
-
Direct Infection: SARS-CoV-2 may directly attack the brain and central nervous system, with symptoms potentially lingering as the body recovers.
Researchers continue investigating these possibilities to better understand the links between COVID-19 and long-term neurological damage.
Certain populations, particularly those with pre-existing conditions like diabetes or heart disease, may be at higher risk. However, more research is needed to confirm specific risk factors for brain-related complications after COVID-19.
COVID-19 Prevention Remains Crucial
Given the evidence, preventing COVID-19 infection is vital for preserving brain health. Following recommended precautions, staying up-to-date on vaccinations, and maintaining healthy lifestyle habits are essential strategies.
Vaccination has been shown to reduce the risk of developing long COVID symptoms—including neurological ones—by about 20%, though vaccines alone are not a complete safeguard.
Currently, there is no proven method to completely prevent neurological issues after infection. However, early treatment of COVID-19 with therapies like Paxlovid, and careful management of chronic conditions, may help reduce risks.
"If you develop lingering symptoms after COVID, seek medical advice," said Karen Hirsch, MD, a neurologist at Stanford Health Care. "Staying healthy, active, and working closely with your healthcare provider is critical."
Although many questions remain, continued research offers hope for better prevention and treatment strategies in the future.
"We urgently need to understand the biological mechanisms," said Dr. Al-Aly. "Only then can we develop effective ways to protect brain health in the aftermath of COVID-19."












.png)




.png)







.webp)
.webp)


.png)